Newly found mechanism can supercharge the immune system against cancers
2025-08-04T11:35:00+10:00

New research could pave the way for more personalised, effective immunotherapy treatments against a range of cancers.
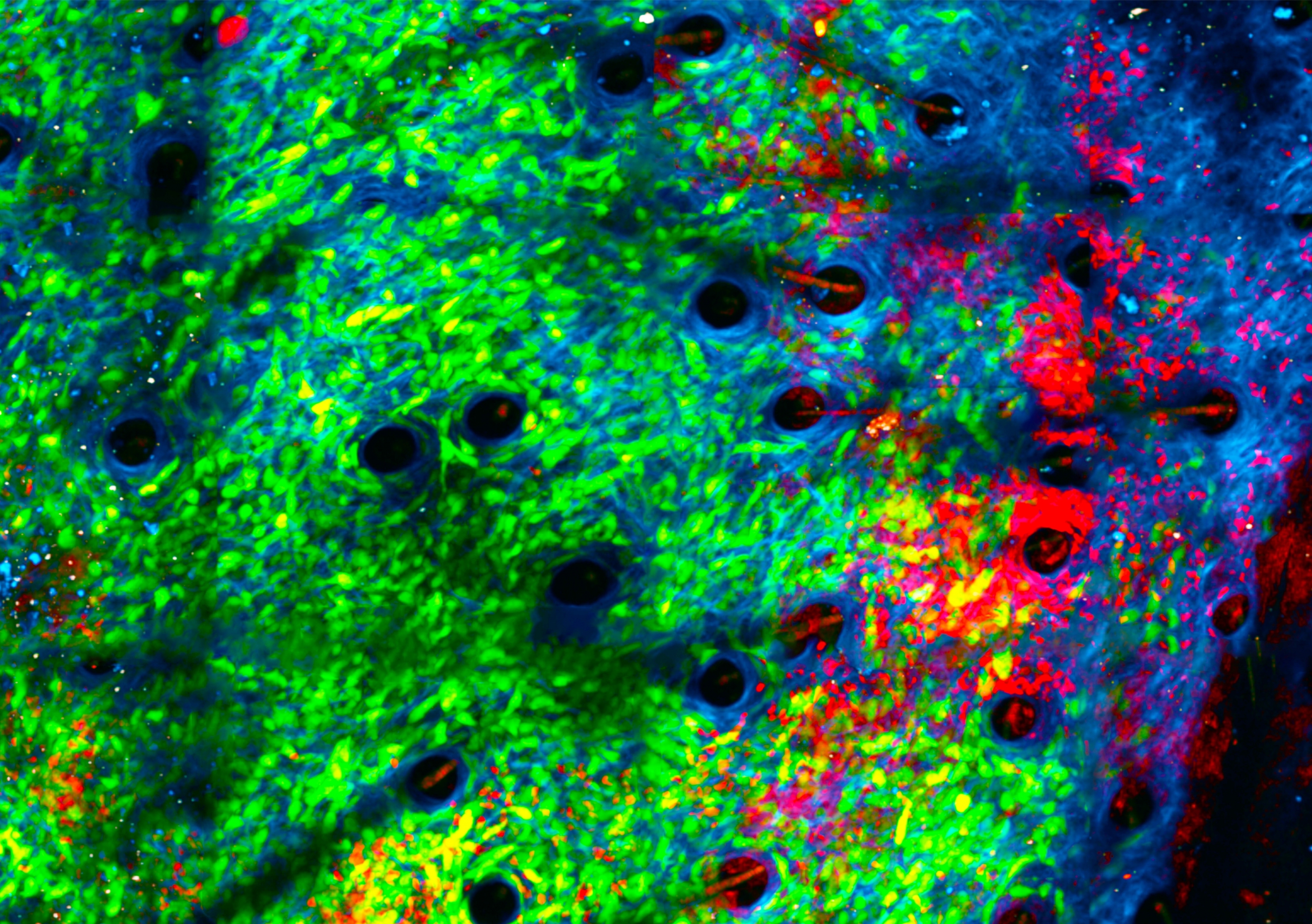
Photo: Adobe Stock
Researchers have discovered new pathways that may explain differences in the way people with cancer respond to immunotherapy.
New research has uncovered a novel mechanism that may help explain why some people with cancer respond remarkably well to immunotherapy while others donÔÇÖt.┬á┬á
Researchers from the and ▓¦¦«╩ËãÁ Sydney have uncovered that less active versions of a gene called NOD2, in combination with radiotherapy or immunotherapy, may help supercharge the immune systemÔÇÖs ability to attack cancer.┬á
The findings, published in the journal , could pave the way for more personalised and effective immunotherapy treatments against a range of cancers. 
Immunotherapy fights cancer, but not everyone responds equally 
Immunotherapy has emerged as one of the most significant advances in cancer treatment in recent decades. It works by recruiting the bodyÔÇÖs immune system to recognise and eliminate cancer cells. But not everyone responds equally, with some experiencing strong immune activation, while others experience no effect.┬á
One widely used cancer immunotherapy is called anti-PD1, part of a family of treatments called checkpoint inhibitors. Normally, cancer evades elimination by the immune system by putting a brake on the action of immune cells. Checkpoint inhibitors release this brake, allowing the immune system to see and destroy cancer cells. 
Anti-PD1 therapy is now commonly used for treating many cancers, including lung, skin, blood and gastrointestinal cancers. 
ÔÇ£Anti-PD1 therapy has become part of standard treatment for many cancers. But only a minority of people experience a really significant benefit, and we donÔÇÖt completely understand why,ÔÇØ says ▓¦¦«╩ËãÁ Conjoint Associate Professor a clinician researcher at Garvan and co-lead of the study.
Media enquiries
For enquiries about this story and interview requests, please contact┬áKate Burke, News & Content Coordinator, ▓¦¦«╩ËãÁ Medicine & Health.
░ı▒▒¶:╠²+61 2 9348 2538
Àí│¥▓╣¥▒▒¶:╠²kate.burke@unsw.edu.au
A new mechanism to boost immunotherapy
To understand why some people respond well to anti-PD1 and others donÔÇÖt, researchers studied a group of people who responded exceptionally well to this therapy.
From a group of 742 Australians with the most common form of advanced lung cancer who underwent treatment with anti-PD1, the team identified 40 whose immune system responded very well, as seen by longer survival accompanied by autoimmune reactions. When the researchers analysed their inherited genes, they found they were more than twice as likely as the general population to have less active versions of a gene called NOD2, in combination with an autoimmune type reaction caused by the immunotherapy.
ÔÇ£This suggests that blocking two different mechanisms, one governed by PD1 and the other by NOD2, combines to supercharge the immune system against cancer cells. This was a surprising finding and points to the marvel and complexity of the immune system,ÔÇØ says study co-lead Professor┬áChris Goodnow, Laboratory Head at Garvan and Professor in the┬á╠²▓╣▓È╗Õ╠²School of Biomedical Sciences┬áat ▓¦¦«╩ËãÁ.
Encouragingly, the immune-boosting effect of NOD2 was not limited to lung cancer. The team showed that in 160 people with a range of cancers who had undergone anti-PD1 treatment, those who had less active versions of NOD2 showed a better response to the therapy. Furthermore, the role of the NOD2 pathway in immunotherapy response was confirmed in preclinical models of colorectal cancer.
ÔÇ£These findings are important because they help us understand the role of the patient as well as the cancer in responding to immune therapy,ÔÇØ says A/Prof. Barnet. ÔÇ£Less active versions of the immune regulator gene NOD2 are often found in people with CrohnÔÇÖs disease, an autoinflammatory condition of the gut. This was the first time that the gene has been identified as playing a role in anti-cancer response to immunotherapy.ÔÇØ
Prof. Goodnow adds: ÔÇ£We believe that for those people undergoing anti-PD1 therapy and experiencing an autoimmune-like response to the treatment, having less active NOD2 gives the immune system an additional nudge to attack and eliminate cancer cells. This is exciting as it suggests that the action of immunotherapies could be boosted through several complementary pathways.ÔÇØ
The importance of understanding exceptional responses to therapy
The team is now investigating ÔÇÿexceptional respondersÔÇÖ ÔÇô both people who respond very well or very poorly to treatment ÔÇô across a variety of cancers and therapies. This is an established research led by the Garvan.
Prof. Goodnow states: ÔÇ£Building on the success of the exceptional responder approach, A/Prof. Barnet and the team is expanding its focus to study different cancers and treatments including chemotherapy. Our aim is to better predict therapeutic responses, to deliver a more personalised approach to cancer treatment, and in turn achieve better outcomes for people with cancer.ÔÇØ
This research was supported through an NHMRC Investigator Grant, the Bill and Patricia Ritchie Foundation Chair in Immunogenomics and the Exceptional Responders Program from Bioplatforms Australia and the Kinghorn Foundation.